Abstract
Introduction: Luminal gastrointestinal tract cancers (LGC) comprise an epidemiologically large burden of disease. Variability in outcomes exists based on the primary site and stage of disease, and many patients with LGC can be achieve long-term responses with surgery, cytotoxic and/or targeted therapies, and radiation. As advances have been made, especially in the molecular profiling and targeting of these tumors, overall survival has been prolonged (Hu, et al. 2015). Many therapies used to treat LGC have the potential for bone marrow toxicity, placing patients at risk of developing therapy-related myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML). Despite this, subsequent myeloid malignancies (MyM), whether definitively treatment-related or not, have not been comprehensively studied or described. We conducted a single-institution review of patients who underwent evaluation for a MyM who had previously been diagnosed with an LGC, expanding a cohort from our same institution (Stein, et al. 2012).
Methods: We identified all patients (N = 6,042) evaluated for MyM - MDS (including chronic myelomonocytic leukemia and MDS-myeloproliferative neoplasm overlap) or AML (including acute promyelocytic leukemia), in which the same patient had a diagnosis code corresponding to an LGC (esophagus, stomach, small and large bowel/rectum, and anus). Patients were excluded if the LGC was lymphoma or stromal tumor. Patient, disease, and treatment information was extracted for analysis. Cytogenetic risk profiles were designated according to the Revised International Prognostic Scoring System for MDS (Greenberg, et al. 2012) and the European LeukemiaNet Guidelines for AML (Döhner, et al. 2016). A Wilcoxon rank sum test was performed to compare latency periods between patients who underwent surgery alone and all others with known treatments.
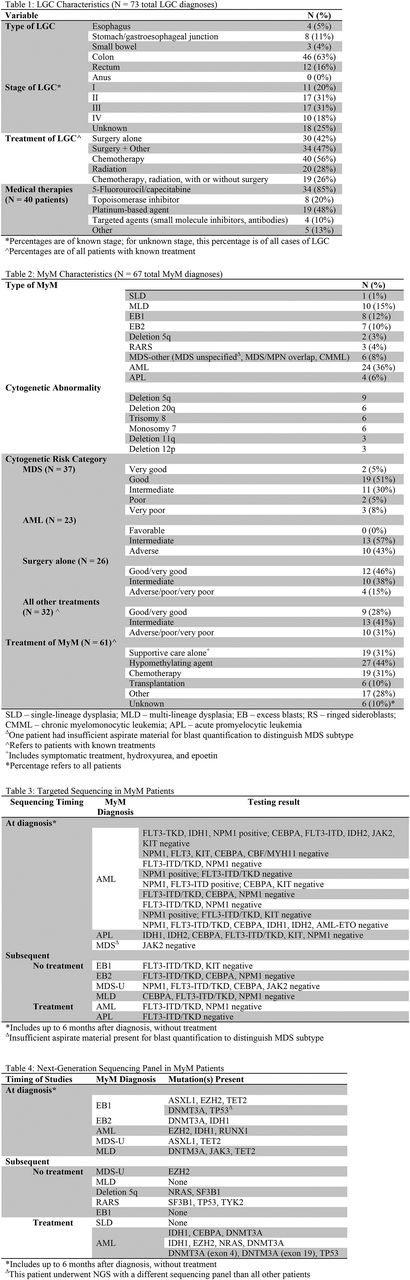
Results: A total of 67 patients (1% of all MyM patients) were included in our cohort, including 73 LGC diagnoses, with four patients having multiple LGCs. The mean age at diagnosis of MyM was 70 years (SD = 11), with median duration between initiation of treatment of LGC and diagnosis MyM of 8.9 years (SD = 8.6). For patients who underwent surgery alone, the mean latency period was 12.9 years (SD = 11.1), compared to all other treatments being 6.1 years (SD = 4.7, p=0.02). The most common LGC was colon (46 cases, 63%) and the most common MyM was AML (36%); 18 patients (27%) had another cancer besides LGC prior to diagnosis of MyM, one of whom received chemotherapy. Table 1 displays LGC treatment characteristics: the majority of cases were treated with surgery (64 patients, 89%), and many with chemotherapy, most commonly 5-fluorourocil or capecitabine (34 patients) followed by platinum compounds (19 patients). A minority, 43% underwent surgery alone, and 28% received radiation therapy. Examining MyM characteristics, 60 patients (96%) had cytogenetic information available at time of diagnosis. Intermediate or adverse cytogenetic risk was common, occurring in 43% of MDS patients and 100% of AML patients; del(5q) was the most common cytogenetic abnormality overall. 35 patients had sequencing data available: 21 patients with targeted testing, 14 with a 49-gene next-generation (NGS) PCR panel, and one patient with sequencing from a different panel. Tables 3 and 4 display full sequencing results. DNMT3A mutations were most common (6 patients with 7 mutations), followed by IDH1 (5 patients); 13 patients had more than one mutation present. Median overall survival after diagnosis of MyM was 15.6 months (95% CI: 10.1-30.5), and the most common treatment was hypomethylating agents (27 patients, 44% among those with treatment information).
Conclusions:Among patients diagnosed with MyM following LGC, a high proportion harbored cytogenetic changes. There was a trend towards a shorter latency period among patients who received treatments besides surgery alone for LGC. Deletion 5q and mutated DNTM3A (testing mostly limited to patients with NGS performed) were the most common abnormalities identified. Given the high incidence of LGC and recent improvements in survival for these patients, future studies should further investigate the incidence of subsequent MyM, risk factors therein, the potential role, if any, for platinum agents in this process, and clinical outcomes. The significance of specific molecular aberrations in this population remains undefined.
Stein: Novartis: Consultancy, Research Funding; Constellation Pharma: Research Funding; Agios Pharmaceuticals, Inc.: Consultancy, Research Funding; Celgene Corporation: Consultancy, Other: Travel expenses, Research Funding; Pfizer: Consultancy, Other: Travel expenses; GSK: Other: Advisory Board, Research Funding; Seattle Genetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal